Understanding the Ethics of Human Experimentation
The realm of human experimentation is a fascinating yet complex area that intertwines the pursuit of scientific knowledge with profound ethical considerations. As we delve into this topic, it's essential to grasp the delicate balance between advancing medical science and upholding the rights and dignity of individuals. Throughout history, human experimentation has played a pivotal role in the development of medical practices and treatments, but it has also been marred by instances of abuse and exploitation. The lessons learned from these historical missteps have shaped the ethical frameworks we rely on today.
The ethical landscape surrounding human experimentation is not just about adhering to rules; it’s about fostering a culture of respect and responsibility towards participants. Researchers must navigate a myriad of ethical principles that guide their conduct, ensuring that the quest for knowledge does not come at the expense of human rights. This article aims to explore these ethical considerations, starting with the historical context that has influenced current practices, followed by the key ethical principles that govern research, and the regulatory frameworks designed to protect human subjects.
As we venture through this discussion, consider the implications of human experimentation in your life. Have you ever participated in a study? Did you know what you were signing up for? These questions are vital in understanding the importance of informed consent and the ethical obligations researchers owe to their participants. The balance between scientific advancement and ethical integrity is not merely a theoretical debate; it affects real lives and shapes the future of medical research.
Moreover, the exploration of vulnerable populations within research highlights the necessity of additional safeguards. These groups may include children, the elderly, or those with cognitive impairments, all of whom require a heightened level of protection to ensure their rights and well-being are not compromised. The ethical dilemmas faced in human experimentation compel us to reflect on our values and the impact of our decisions on the lives of others.
In this article, we will also dissect various case studies that exemplify the consequences of neglecting ethical standards. From the infamous Tuskegee Syphilis Study to the controversial Stanford Prison Experiment, these examples serve as powerful reminders of the potential for harm when ethical considerations are sidelined. As we navigate through these narratives, we will uncover the lessons learned and the ongoing challenges that researchers must confront to ensure ethical integrity in their work.
Finally, to enhance your understanding, we will include a Frequently Asked Questions section at the end of this article. This will address common queries related to the ethics of human experimentation, ensuring that you leave with a comprehensive grasp of this vital topic. So, let’s embark on this journey to understand the ethics of human experimentation, a journey that is as important as the scientific discoveries it aims to support.
The Historical Context of Human Experimentation
The journey of human experimentation is as complex as it is fascinating, weaving through the fabric of history and science. From the early days of rudimentary medical practices to the advanced clinical trials we see today, the evolution of ethical standards has been shaped by significant events that have left a lasting impact on research involving human subjects. In the past, experimentation was often conducted without the consent or knowledge of participants, leading to numerous ethical violations and abuses. For instance, during the 19th century, medical practitioners often used patients in asylums or hospitals as subjects for experiments, frequently without any regard for their rights or well-being.
One of the pivotal moments in this history was the aftermath of World War II, which exposed horrific human rights violations conducted under the guise of medical research. The Nuremberg Trials brought to light the atrocities committed by Nazi doctors, leading to the establishment of the Nuremberg Code in 1947. This code laid down ten principles that emphasized the necessity of voluntary consent and the importance of minimizing harm to participants. It was a watershed moment that prompted a global reevaluation of ethical standards in human experimentation.
Another significant milestone occurred in the 1960s and 1970s with the emergence of various social movements advocating for civil rights, patient rights, and ethical accountability in medicine. The Belmont Report, published in 1979, further solidified the ethical framework for research involving human subjects by introducing three foundational principles: respect for persons, beneficence, and justice. These principles have since become cornerstones in the ethical conduct of research, guiding researchers to prioritize the rights and welfare of participants.
As we delve deeper into the historical context, it’s important to recognize that the evolution of human experimentation ethics is not just a chronological timeline but a reflection of societal values and moral considerations. The lessons learned from past mistakes serve as a reminder of the delicate balance that must be maintained between scientific advancement and the protection of human rights. Today, researchers are held to rigorous ethical standards, and the emphasis on informed consent and participant welfare is paramount. However, the shadows of history still loom large, urging us to remain vigilant against potential abuses in the name of science.
| Event | Year | Significance |
|---|---|---|
| Nuremberg Code Established | 1947 | Set the foundation for ethical standards in human experimentation. |
| Belmont Report Published | 1979 | Introduced key ethical principles guiding research practices. |
| Declaration of Helsinki Adopted | 1964 | Outlined ethical principles for medical research involving human subjects. |
In conclusion, the historical context of human experimentation is a tapestry of lessons learned through both triumphs and tragedies. It serves as a reminder of the importance of ethical considerations in research and the ongoing responsibility of the scientific community to uphold the dignity and rights of all participants. As we move forward, it is crucial to reflect on this history to ensure that the mistakes of the past are not repeated, and that the pursuit of knowledge always respects the humanity of those involved.
- What is informed consent? Informed consent is the process of providing potential research participants with all necessary information about a study, allowing them to make an educated decision about their participation.
- Why is ethical oversight important in research? Ethical oversight is essential to protect the rights and welfare of participants, ensuring that research is conducted responsibly and with respect for human dignity.
- What are vulnerable populations in research? Vulnerable populations include groups who may be at higher risk of exploitation or harm, such as children, prisoners, or individuals with cognitive impairments.

Key Ethical Principles
When it comes to human experimentation, ethical principles serve as the backbone of responsible research. These principles not only guide researchers in their quest for knowledge but also ensure that the rights and dignity of participants are upheld. Let’s dive into some of the core ethical principles that shape the landscape of human experimentation: autonomy, beneficence, non-maleficence, and justice. Each of these principles plays a crucial role in the ethical conduct of research.
Autonomy refers to the right of individuals to make informed decisions about their own lives. In the context of research, this means that participants should have the freedom to choose whether or not to partake in a study, based on a clear understanding of what it entails. Imagine being given a map before embarking on a journey; autonomy is that map, guiding participants through the twists and turns of research involvement. Researchers must respect this autonomy by providing comprehensive information and ensuring that consent is given voluntarily.
Next is beneficence, which emphasizes the obligation of researchers to maximize potential benefits while minimizing any possible harm to participants. It’s like a double-edged sword—while the quest for knowledge is important, it should never come at the cost of a participant's well-being. Researchers must weigh the potential benefits of their studies against the risks involved, striving to create a balance that favors the participants. This principle reminds us that every research endeavor should aim to contribute positively to society.
Closely related to beneficence is the principle of non-maleficence, which is perhaps best summed up by the age-old adage, "do no harm." This principle reinforces the idea that researchers must avoid causing physical, psychological, or emotional harm to participants. It’s essential for researchers to assess potential risks and implement safeguards to protect participants from harm. For instance, if a study involves a new drug, researchers must conduct thorough pre-trial assessments to ensure that the drug does not pose undue risks to participants.
Lastly, we have justice, which addresses the fair distribution of the benefits and burdens of research. This principle calls for equitable selection of participants, ensuring that no group is unfairly burdened or excluded from the potential benefits of research. It’s like a balancing act—researchers must ensure that their studies do not disproportionately target vulnerable populations while leaving others untouched. This principle is vital in fostering trust between researchers and communities, ensuring that everyone has a seat at the table.
In summary, these key ethical principles are not just abstract concepts; they are essential guidelines that help researchers navigate the complex landscape of human experimentation. By adhering to autonomy, beneficence, non-maleficence, and justice, researchers can contribute to scientific advancement while respecting the rights and dignity of participants. As we move forward in the realm of research, let’s keep these principles at the forefront, ensuring that human experimentation is conducted ethically and responsibly.
Informed Consent
Informed consent is not just a formality; it's the very backbone of ethical research involving human subjects. Imagine being asked to participate in a study without fully understanding what it entails. It’s like jumping into a pool without knowing if there’s water in it! Informed consent ensures that participants are fully aware of the risks, benefits, and procedures involved before they agree to take part in any research. This process is crucial because it respects the autonomy of individuals, allowing them to make educated decisions about their participation.
The process of obtaining informed consent is not merely about signing a document; it's about fostering a clear and open dialogue between researchers and participants. Researchers must communicate the study's purpose, what is expected from participants, and any potential risks involved. This includes disclosing information about how the data will be used and who will have access to it. Participants should feel comfortable asking questions and expressing concerns. It's essential that they understand that their participation is entirely voluntary and that they can withdraw at any time without any repercussions.
Obtaining informed consent is a multi-step process that requires diligence and care. Here’s how it typically unfolds:
- Information Dissemination: Researchers provide detailed information about the study, including its purpose, duration, procedures, and potential risks.
- Question and Answer Session: Participants are encouraged to ask questions to clarify any doubts they may have.
- Voluntary Participation: It must be made clear that participation is voluntary, and individuals can opt out at any time.
- Documentation: Once participants are fully informed and agree to participate, they provide their consent, typically by signing a consent form.
However, the road to obtaining informed consent isn't always smooth. Researchers often face several challenges that can complicate this essential process.
One of the significant challenges researchers encounter is ensuring that all participants truly understand the information presented to them. Factors such as language barriers can make it difficult for some participants to grasp complex medical or technical terms. Cognitive impairments can further complicate matters, as individuals with certain disabilities may struggle to comprehend the implications of their participation. Moreover, the complexity of study protocols can overwhelm potential participants, making it hard for them to fully understand what they are agreeing to. This is why researchers must be adaptable and patient, often needing to simplify their explanations and provide additional support to ensure clarity.
Informed consent is not just a checkbox to tick off; it's a fundamental ethical obligation that safeguards the rights and dignity of participants. It embodies the principle of respect for persons, ensuring that individuals are treated as autonomous agents capable of making their own choices. By prioritizing informed consent, researchers not only uphold ethical standards but also foster trust and transparency in the research process.
Q1: What is informed consent?
A1: Informed consent is a process through which participants are fully educated about a study's details, including risks and benefits, before agreeing to participate.
Q2: Why is informed consent important?
A2: It ensures that participants have the autonomy to make informed decisions about their involvement in research, protecting their rights and well-being.
Q3: What challenges do researchers face in obtaining informed consent?
A3: Challenges include language barriers, cognitive impairments, and the complexity of study protocols that can confuse participants.
Q4: Can participants withdraw their consent?
A4: Yes, participants can withdraw their consent at any time without facing any negative consequences.

Process of Obtaining Consent
Obtaining informed consent is a fundamental process in ethical research, acting as the bridge between researchers and participants. It's not just a formality; it's a commitment to transparency and respect for individual autonomy. The journey begins with clear communication. Researchers must articulate the purpose of the study, the procedures involved, and any potential risks and benefits in a language that participants can easily understand. Imagine you’re signing up for a thrilling adventure—wouldn’t you want to know what to expect? This is the essence of informed consent.
During this process, it's crucial to create an environment where participants feel comfortable asking questions. Researchers should encourage dialogue, inviting participants to voice their concerns or seek clarification. This two-way communication fosters trust and ensures that consent is not just a checkbox but a genuine understanding of the study. Additionally, it's important to emphasize that participation is entirely voluntary. No one should feel pressured to take part; after all, consent obtained under duress is not consent at all.
To illustrate the process further, consider the following key steps involved in obtaining informed consent:
- Preparation: Researchers should prepare a comprehensive information sheet detailing the study's objectives, methods, and implications.
- Discussion: Engage participants in a conversation about the study, allowing them to ask questions and express any concerns.
- Documentation: Once participants are adequately informed and ready to proceed, obtain their signature on a consent form, ensuring they understand what they are agreeing to.
- Follow-up: After consent is obtained, researchers should maintain open lines of communication, allowing participants to withdraw or ask questions at any point during the study.
However, the process of obtaining consent is not without its challenges. Researchers often encounter barriers such as language differences, cognitive impairments, or complex study protocols that may confuse participants. For instance, if a participant speaks a different language, providing a translated consent form is essential, but it must also be accompanied by a verbal explanation to ensure comprehension. Similarly, when dealing with populations that may have cognitive impairments, researchers must take extra care to simplify information and verify understanding, often involving guardians or advocates in the process.
In conclusion, the process of obtaining informed consent is a critical aspect of ethical research. It goes beyond mere documentation; it is about fostering a respectful relationship between researchers and participants. By prioritizing clear communication, voluntary participation, and ongoing support, researchers can uphold ethical standards and ensure that human subjects are treated with the dignity and respect they deserve.

Challenges in Informed Consent
Obtaining informed consent is a fundamental aspect of ethical research, yet it is not without its challenges. One of the most significant hurdles researchers face is ensuring that participants fully understand the information presented to them. This is particularly crucial when dealing with complex medical terminologies or intricate study protocols. Imagine trying to explain a complicated scientific process to someone without a background in science; it can be daunting. Researchers must break down the information into digestible pieces, ensuring clarity without oversimplifying the content.
Another challenge arises from language barriers. In a diverse world, researchers often engage participants from various linguistic backgrounds. If a participant does not speak the language in which the consent form is written, they may not grasp the risks or benefits involved in the study. This situation can lead to misunderstandings, and ultimately, a lack of true informed consent. To mitigate this, researchers should consider providing consent forms in multiple languages or employing translators to facilitate communication.
Cognitive impairments present another layer of complexity in the informed consent process. Individuals with cognitive disabilities, mental health issues, or age-related conditions may struggle to comprehend the implications of their participation. In these cases, it becomes essential to assess the participant's ability to provide informed consent genuinely. Researchers might need to involve guardians or advocates to ensure that the rights and welfare of these vulnerable individuals are protected. However, this can lead to ethical dilemmas regarding autonomy and the extent to which a participant can make their own decisions.
Moreover, the complexity of study protocols can also hinder understanding. Some studies involve multiple phases, extensive procedures, or long-term commitments that can overwhelm potential participants. Researchers must strive to present this information in a straightforward and engaging manner. Utilizing visual aids, such as charts or infographics, can help convey complicated information more effectively.
Finally, the pressure of participation can create an environment where individuals feel coerced into agreeing. Whether due to financial incentives, social pressure, or a desire to please the researchers, participants may consent without fully understanding what they are agreeing to. This is where the ethical responsibility of researchers comes into play; they must create a supportive atmosphere that encourages questions and allows for genuine voluntary participation.
In summary, while informed consent is a cornerstone of ethical research, various challenges can impede its effectiveness. Researchers must navigate language barriers, cognitive impairments, complex protocols, and potential coercion to ensure that participants are genuinely informed and able to make autonomous decisions. By addressing these challenges thoughtfully, researchers can uphold ethical standards and protect the rights of their participants.
- What is informed consent? Informed consent is the process by which researchers ensure that participants understand the risks, benefits, and procedures involved in a study before agreeing to take part.
- Why is informed consent important? It protects the autonomy of participants and ensures ethical standards are upheld in research.
- What challenges do researchers face in obtaining informed consent? Challenges include language barriers, cognitive impairments, complex study protocols, and potential coercion.
- How can researchers overcome these challenges? By providing clear information, using translators, involving advocates for vulnerable populations, and creating a supportive environment for questions.

Vulnerable Populations
When we talk about in the context of human experimentation, we're diving into a complex and sensitive area of research ethics. Vulnerable populations include groups such as children, the elderly, individuals with cognitive impairments, economically disadvantaged people, and those with limited access to healthcare. These groups often face heightened risks in research settings, not just because of their circumstances, but also due to systemic inequalities that can lead to exploitation. It's crucial to recognize that their participation in research must be approached with an extra layer of caution and care.
Why do we need to be extra vigilant when it comes to these populations? Well, the answer lies in the balance between scientific advancement and ethical responsibility. Researchers must ensure that they’re not just seeking to advance knowledge or develop new treatments at the expense of those who are most vulnerable. The ethical principle of justice comes into play here, ensuring that the benefits and burdens of research are distributed fairly among all groups in society. This means that vulnerable populations should not be disproportionately burdened by research risks while receiving little to no benefit from the outcomes.
For instance, consider a clinical trial for a new medication aimed at treating a specific disease that primarily affects low-income communities. If researchers fail to provide adequate protections or informed consent processes tailored to these populations, they risk not only ethical violations but also the integrity of the research itself. Participants must understand not only the potential benefits but also the risks involved, and this communication must be clear and accessible.
Moreover, researchers must implement additional safeguards to protect these groups. This can include:
- Ensuring that consent forms are written in plain language.
- Providing additional support during the consent process, such as the presence of advocates or translators.
- Conducting ongoing assessments of the risks faced by participants throughout the study.
It’s also essential to involve community representatives in the research design and implementation phases. This ensures that the needs and concerns of vulnerable populations are addressed, fostering a sense of trust and collaboration between researchers and participants. By doing this, researchers not only uphold ethical standards but also enhance the quality and applicability of their findings.
In summary, protecting vulnerable populations in human experimentation is not just a regulatory requirement; it’s a moral imperative. As we continue to push the boundaries of scientific research, we must remain committed to ethical practices that respect the dignity and rights of all participants. Only then can we ensure that our quest for knowledge does not come at the expense of those who are most at risk.
- What defines a vulnerable population?
Vulnerable populations are groups that may be at increased risk of harm or exploitation in research settings, including children, the elderly, and those with cognitive impairments. - Why is informed consent particularly important for vulnerable populations?
Informed consent ensures that participants understand the risks and benefits of their involvement, which is crucial for protecting those who may not fully comprehend the implications of the research. - How can researchers ensure ethical treatment of vulnerable populations?
Researchers can implement additional safeguards, involve community representatives, and ensure clear communication throughout the research process.

Regulatory Frameworks
The landscape of human experimentation is not just shaped by the ethical principles that guide researchers but also by a robust set of designed to protect human subjects. These frameworks are crucial in ensuring that research is conducted responsibly while respecting the rights and dignity of participants. Over the years, various organizations and governing bodies have established guidelines that serve as a foundation for ethical research practices. Understanding these regulations is essential for anyone involved in human research, whether they are researchers, participants, or policymakers.
One of the most significant documents in this realm is the Declaration of Helsinki, developed by the World Medical Association. This declaration outlines ethical principles for medical research involving human subjects, emphasizing the necessity of informed consent and the welfare of participants. It serves as a guiding beacon for researchers around the globe, ensuring that the dignity and rights of individuals are prioritized. Similarly, the Belmont Report, issued by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research in the United States, outlines foundational ethical principles that include respect for persons, beneficence, and justice. These documents collectively create a framework that not only guides research practices but also fosters public trust in scientific endeavors.
In addition to these foundational documents, various regulatory bodies and Institutional Review Boards (IRBs) play a vital role in overseeing research activities. IRBs are responsible for reviewing research proposals to ensure that they meet ethical standards and that the rights and welfare of participants are safeguarded. They assess the risk-to-benefit ratio of studies, ensuring that any potential harm to participants is minimized and justified by the anticipated benefits of the research. This review process is essential in maintaining ethical integrity in human experimentation.
Moreover, international regulations are increasingly important as research transcends borders. The International Conference on Harmonisation (ICH) has established guidelines that aim to ensure that drug development and clinical trials are conducted ethically and efficiently across different countries. These guidelines help create a standardized approach to research ethics, promoting respect for individuals and fair treatment across diverse populations.
As we navigate through the complexities of human research, the importance of these regulatory frameworks cannot be overstated. They serve not only as a safeguard for participants but also as a roadmap for researchers, guiding them in their quest for knowledge while ensuring that ethical standards are upheld. Without these regulations, the potential for abuse and exploitation in human experimentation would significantly increase, undermining the very foundation of scientific inquiry.
In conclusion, the regulatory frameworks surrounding human experimentation are essential for balancing scientific advancement with the protection of human rights. As research practices continue to evolve, so too must these frameworks, adapting to new challenges and ensuring that ethical standards remain at the forefront of human experimentation.
- What is the purpose of regulatory frameworks in human experimentation? Regulatory frameworks ensure the protection of human subjects, promote ethical research practices, and maintain public trust in scientific endeavors.
- What role do Institutional Review Boards (IRBs) play? IRBs review research proposals to ensure ethical standards are upheld and that participants' rights and welfare are safeguarded.
- How do international regulations impact human research? International regulations provide standardized guidelines for ethical research practices, promoting respect for individuals and fair treatment across borders.

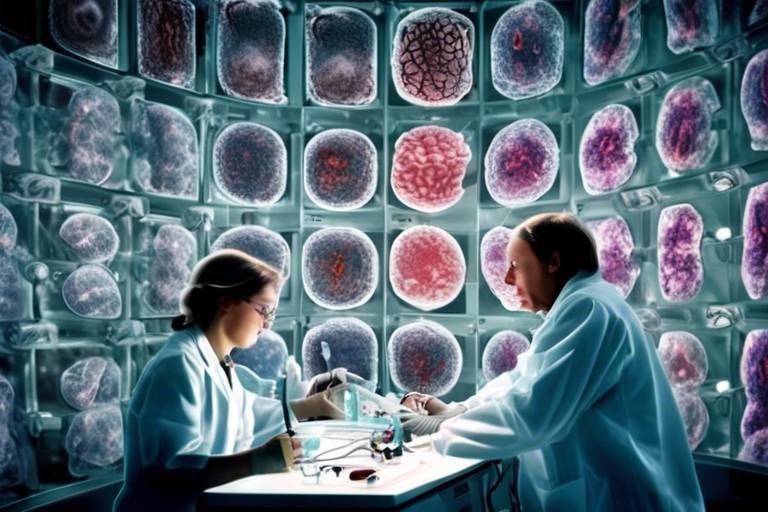
Institutional Review Boards (IRBs)
Institutional Review Boards, commonly known as IRBs, are a fundamental component in the landscape of ethical human research. These boards are established within various institutions, including universities and hospitals, to ensure that all research involving human subjects adheres to ethical standards and regulations. The primary role of an IRB is to review research proposals and assess their potential risks and benefits, ensuring that the rights and welfare of participants are protected. This oversight is crucial, as it acts as a safeguard against unethical practices that have occurred in the past.
When a researcher submits a proposal, the IRB conducts a thorough evaluation that encompasses several key factors. For instance, they will assess the scientific validity of the study, ensuring that the research questions posed are not only meaningful but also justifiable. Moreover, the IRB examines the methods proposed for data collection and participant engagement, ensuring that they are ethical and appropriate. This includes a careful look at how informed consent will be obtained, which is a crucial aspect of ethical research.
IRBs are composed of a diverse group of individuals, often including scientists, ethicists, and community representatives. This diversity helps to bring multiple perspectives to the review process, ensuring that the interests of various stakeholders are considered. The presence of lay members is particularly important, as they can provide insight into how the research might be perceived by the general public, thereby enhancing the ethical scrutiny of the proposals.
The IRB process typically involves several stages, including:
- Initial Review: The IRB conducts a comprehensive review of the research proposal, evaluating the risks to participants against the potential benefits of the research.
- Ongoing Monitoring: Once a study is approved, the IRB continues to monitor the research to ensure compliance with ethical standards throughout the study's duration.
- Reporting and Review: Any adverse events or changes in the study must be reported to the IRB, which will reassess the ethical implications of the research.
Furthermore, IRBs have the authority to approve, require modifications to, or disapprove research proposals based on their ethical considerations. This power is not just a formality; it plays a critical role in maintaining public trust in research practices. By ensuring that human rights are respected, IRBs contribute significantly to the integrity of the scientific community.
In conclusion, Institutional Review Boards are indispensable in the realm of human experimentation. They serve as watchdogs, ensuring that research is conducted ethically and responsibly. Their role in reviewing proposals, monitoring ongoing studies, and protecting participants cannot be overstated. As we move forward in the era of advanced research methodologies, the importance of IRBs will continue to grow, emphasizing the need for ethical vigilance in all human research endeavors.
What is the primary function of an IRB?
The primary function of an IRB is to review research proposals involving human subjects to ensure ethical standards are met and that participants' rights and welfare are protected.
Who serves on an IRB?
An IRB typically consists of a diverse group of individuals, including scientists, ethicists, legal experts, and community representatives, to provide a well-rounded perspective on ethical issues.
What happens if an IRB disapproves a research proposal?
If an IRB disapproves a research proposal, the researchers must address the concerns raised by the board, make necessary modifications, and resubmit the proposal for further review.
How does an IRB ensure informed consent?
An IRB ensures informed consent by reviewing the methods proposed for obtaining consent, verifying that participants are fully informed of the risks, benefits, and procedures before agreeing to participate.

International Regulations
International regulations play a pivotal role in shaping the ethical landscape of human experimentation. These guidelines are designed to protect the rights and welfare of research participants, ensuring that studies conducted across borders adhere to universally accepted ethical standards. One of the most influential documents in this realm is the Belmont Report, which outlines fundamental ethical principles that should govern research involving human subjects. The Belmont Report emphasizes three key principles: respect for persons, beneficence, and justice. These principles serve as a foundation for many international regulations and ethical guidelines today.
The Declaration of Helsinki, developed by the World Medical Association, is another significant international guideline that researchers must consider. It provides a comprehensive framework for conducting medical research involving human subjects, emphasizing the necessity of informed consent and the importance of assessing risks and benefits. The Declaration of Helsinki has undergone several revisions since its inception in 1964, reflecting the evolving nature of ethical considerations in research and the need for continual reassessment of ethical standards.
Moreover, organizations such as the World Health Organization (WHO) have established ethical guidelines to ensure that research conducted in diverse global contexts respects the rights and dignity of participants. These regulations are particularly important in low-resource settings where ethical oversight may be less stringent. By promoting ethical research practices, these international regulations aim to foster trust between researchers and participants, ultimately enhancing the quality and integrity of scientific research.
In addition to these foundational documents, many countries have their own regulatory frameworks that align with international standards. For instance, the U.S. Department of Health and Human Services has established regulations known as 45 CFR 46 that govern the protection of human subjects in research. These regulations require institutions to obtain Institutional Review Board (IRB) approval before initiating research involving human participants, ensuring that ethical considerations are rigorously evaluated.
In summary, international regulations serve as a critical safeguard in the realm of human experimentation. They not only protect participants but also enhance the credibility of research findings. As science continues to advance, the ongoing dialogue surrounding these regulations will be essential in addressing new ethical challenges that arise in the pursuit of knowledge.
- What is the Belmont Report?
The Belmont Report is a foundational document that outlines ethical principles for research involving human subjects, focusing on respect for persons, beneficence, and justice.
- Why is informed consent important?
Informed consent ensures that participants understand the risks and benefits of a study, allowing them to make an educated decision about their participation.
- What role do Institutional Review Boards (IRBs) play?
IRBs are responsible for reviewing research proposals to ensure that ethical standards are met and that the rights and welfare of participants are protected.
- How do international regulations affect research?
International regulations provide guidelines that researchers must follow to ensure ethical practices, protecting participants and enhancing the integrity of research.

Case Studies in Human Experimentation
Examining case studies in human experimentation provides a sobering look at the ethical dilemmas that have arisen throughout history. These stories not only highlight the potential for scientific advancement but also serve as stark reminders of the consequences of neglecting ethical standards. One of the most notorious examples is the Tuskegee Syphilis Study, which ran from 1932 to 1972. In this study, African American men with syphilis were misled into believing they were receiving treatment, while in reality, they were being observed without consent. This egregious violation of trust and ethics raises critical questions about the sanctity of informed consent and the moral obligations researchers have towards their subjects.
The Stanford Prison Experiment, conducted in 1971, is another compelling case that illustrates the ethical complexities inherent in psychological research. Participants were assigned roles as either guards or prisoners in a simulated prison environment, leading to extreme psychological stress and abusive behavior. The experiment was terminated after only six days, despite being planned for two weeks, due to the alarming reactions observed. This case underscores the ethical challenges associated with deception and the potential for harm in psychological studies. It prompts us to consider: how far is too far when it comes to exploring the depths of human behavior?
Both of these cases serve as cautionary tales that remind us of the necessity for stringent ethical standards in research. They compel us to ask important questions about the balance between scientific inquiry and human rights. As we navigate the complexities of modern research, it is essential to remember the lessons learned from these historical examples. Researchers today must prioritize transparency, informed consent, and the welfare of participants to ensure that history does not repeat itself.
- What is informed consent? Informed consent is the process through which participants are provided with clear information about a study's purpose, procedures, risks, and benefits, allowing them to make an educated decision about their participation.
- Why are vulnerable populations a focus in human experimentation ethics? Vulnerable populations may face increased risks of exploitation or harm, and special considerations are needed to protect their rights and welfare in research.
- What role do Institutional Review Boards (IRBs) play? IRBs review research proposals to ensure that ethical standards are upheld, safeguarding the rights and welfare of participants involved in studies.

The Tuskegee Syphilis Study
The Tuskegee Syphilis Study, conducted between 1932 and 1972, is one of the most notorious examples of unethical human experimentation in history. This study aimed to observe the natural progression of untreated syphilis in African American men. However, what began as a research initiative quickly devolved into a shocking violation of human rights, highlighting the dire consequences of neglecting ethical standards in medical research.
Initially, the study involved 600 men, 399 of whom had syphilis and 201 who were healthy. These men were told they were receiving free healthcare from the U.S. Public Health Service, but in reality, they were misled and not given adequate treatment even after penicillin became the standard cure for syphilis in the 1940s. Instead of helping them, researchers continued to observe their conditions, documenting the disease's progression while denying them the treatment they desperately needed.
The ethical breaches in the Tuskegee Study are staggering. Participants were not informed of their diagnosis, nor were they given the opportunity to consent to the study based on an understanding of their situation. This lack of informed consent is a fundamental violation of the ethical principle of autonomy. The men were treated as mere subjects for observation rather than individuals deserving of care and respect.
Moreover, the study exploited the vulnerabilities of its participants, many of whom were poor and lacked access to quality healthcare. The researchers took advantage of the socio-economic conditions of these men, perpetuating a cycle of exploitation that raises serious questions about justice in medical research. The ethical implications of the Tuskegee Study extend beyond its immediate consequences; it has left a lasting scar on the relationship between the African American community and medical institutions.
In response to the public outcry that followed the revelation of the study in the early 1970s, significant changes were made in the field of research ethics. The Tuskegee Syphilis Study serves as a cautionary tale, reminding us of the critical importance of ethical standards and the necessity of informed consent in research involving human subjects. It emphasizes that scientific advancement must never come at the cost of human dignity and rights.
To further understand the implications of this study, let’s summarize key points in the table below:
| Key Aspect | Description |
|---|---|
| Duration | 1932 - 1972 |
| Participants | 600 African American men (399 with syphilis, 201 without) |
| Misleading Information | Participants were told they were receiving free healthcare |
| Ethical Violations | Lack of informed consent, exploitation of vulnerable populations |
| Consequences | Significant changes in research ethics and regulations |
Ultimately, the Tuskegee Syphilis Study is a stark reminder that ethical considerations are paramount in human experimentation. It compels us to reflect on the importance of treating research participants with respect and dignity, ensuring that their rights are protected, and that they are fully informed about the studies in which they participate.
- What was the purpose of the Tuskegee Syphilis Study?
The study aimed to observe the natural progression of untreated syphilis in African American men. - How long did the study last?
The study lasted for 40 years, from 1932 to 1972. - What were the ethical violations in this study?
Participants were misled, not given informed consent, and denied treatment even after effective options became available. - What impact did the study have on research ethics?
The Tuskegee Study led to significant changes in ethical standards and regulations regarding informed consent and the treatment of research participants.

The Stanford Prison Experiment
The Stanford Prison Experiment is one of the most infamous studies in the history of psychology, conducted by psychologist Philip Zimbardo in 1971. This groundbreaking yet controversial experiment aimed to explore the psychological effects of perceived power by simulating a prison environment. Participants were randomly assigned roles of either guards or prisoners, and what unfolded over a mere six days was nothing short of shocking. The rapid transformation of ordinary college students into abusive guards and submissive prisoners raised profound ethical questions about the limits of human behavior and the responsibilities of researchers.
Initially, the study was intended to last two weeks, but it was abruptly terminated due to the extreme and distressing behavior exhibited by the participants. The guards, who were given uniforms and sunglasses to create a sense of authority, began to exhibit increasingly aggressive and dehumanizing behavior towards the prisoners. The prisoners, on the other hand, quickly succumbed to feelings of helplessness and despair. This dramatic shift highlights the power of situational factors and the ease with which individuals can adopt roles that contradict their personal morals and ethics.
One of the most alarming aspects of the Stanford Prison Experiment was the lack of informed consent regarding the psychological risks involved. While participants were aware they were part of a psychological study, they could not fully comprehend the potential for emotional and psychological distress. Zimbardo himself, who acted as the prison superintendent, became so immersed in the role that he lost sight of his ethical obligations, raising critical questions about the researcher’s duty to protect participants from harm.
In light of these events, the Stanford Prison Experiment serves as a cautionary tale about the ethical implications of psychological research. It compels us to reflect on the following key points:
- Informed Consent: Participants must be fully aware of the potential risks and the nature of the study.
- Researcher Responsibility: Researchers must prioritize the well-being of participants over the pursuit of knowledge.
- Debriefing: Post-experiment debriefing is essential to address any psychological harm caused during the study.
In conclusion, the Stanford Prison Experiment not only sheds light on the darker aspects of human nature but also serves as a pivotal moment in the evolution of ethical standards in research. It reminds us that while the quest for knowledge is vital, it should never come at the expense of human dignity and well-being. The lessons learned from this experiment continue to resonate in the fields of psychology, ethics, and research methodology, urging future researchers to tread carefully and uphold the highest ethical standards.
- What was the main purpose of the Stanford Prison Experiment? The main purpose was to investigate the psychological effects of perceived power and authority in a simulated prison environment.
- How long did the Stanford Prison Experiment last? Although it was intended to last two weeks, the experiment was terminated after just six days due to ethical concerns.
- What ethical issues arose from the Stanford Prison Experiment? Key ethical issues included lack of informed consent, psychological harm to participants, and the failure of researchers to intervene when harm occurred.
- What impact did the Stanford Prison Experiment have on research ethics? The experiment led to stricter ethical guidelines for psychological research, emphasizing the importance of participant welfare and informed consent.
Frequently Asked Questions
- What is human experimentation?
Human experimentation refers to research conducted with human subjects to gather data on health, medicine, and psychology. It can range from clinical trials for new drugs to psychological studies examining behavior.
- Why is informed consent important in research?
Informed consent is crucial because it ensures that participants understand the risks, benefits, and procedures of a study before agreeing to take part. It respects their autonomy and right to make informed decisions about their involvement.
- What are the key ethical principles guiding human experimentation?
The main ethical principles include autonomy (respecting individual choices), beneficence (maximizing benefits while minimizing harm), non-maleficence (avoiding harm), and justice (ensuring fair treatment and distribution of research benefits and burdens).
- How do researchers obtain informed consent?
Researchers obtain informed consent by providing clear information about the study, allowing participants to ask questions, and ensuring that their participation is voluntary and free from coercion.
- What challenges do researchers face in obtaining informed consent?
Common challenges include language barriers, cognitive impairments of participants, and the complexity of study protocols, which can make it difficult for individuals to fully understand what they are agreeing to.
- Who are considered vulnerable populations in research?
Vulnerable populations include groups such as children, elderly individuals, those with cognitive impairments, and economically disadvantaged individuals. Extra precautions are necessary to protect these individuals from exploitation or harm.
- What role do Institutional Review Boards (IRBs) play?
IRBs review research proposals to ensure they meet ethical standards, safeguarding the rights and welfare of participants. They assess risks and benefits, ensuring that research is conducted responsibly.
- What are some international regulations governing human experimentation?
International regulations, such as the Belmont Report, outline ethical principles for conducting research across borders, promoting respect for individuals and ensuring fair treatment in studies globally.
- Can you give an example of a historical case study in human experimentation?
One infamous case is the Tuskegee Syphilis Study, which highlighted the importance of informed consent and ethical treatment. Participants were misled and denied treatment, demonstrating the dire consequences of neglecting ethical standards.
- What lessons can we learn from the Stanford Prison Experiment?
The Stanford Prison Experiment illustrates how situational factors can influence human behavior and raises significant ethical questions about the use of deception and the potential for psychological harm in research.