Philosophy in the Study of Immunology
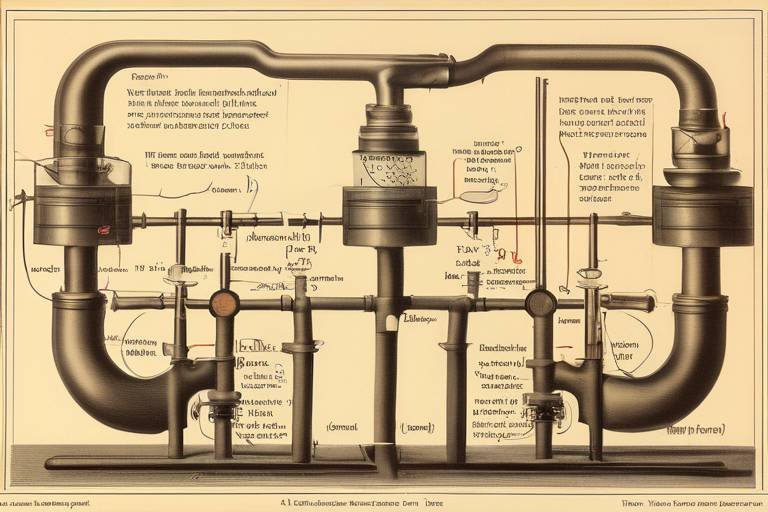
The intersection of philosophy and immunology is a fascinating realm where abstract concepts meet the concrete realities of our immune systems. At first glance, these two fields may seem worlds apart, but they are intricately connected in ways that shape our understanding of health and disease. Just as a painter uses a palette of colors to create a masterpiece, philosophers use their ideas to color our comprehension of the biological processes that protect us from illness. This exploration dives deep into how philosophical inquiry influences immunology, particularly in defining concepts like self and non-self, which are fundamental to understanding immune responses. Imagine a vigilant gatekeeper at the entrance of a castle, distinguishing between friends and foes; this is akin to how our immune system identifies what belongs to the body and what does not.
As we peel back the layers of immunology, we uncover that philosophical questions about identity, agency, and moral responsibility are not just abstract musings but are critical in shaping research and public health policies. The ethical implications of immunological research reflect our values and beliefs, compelling us to consider not only the science but also the human experience behind it. For instance, how do we balance the need for scientific advancement with the rights of individuals participating in clinical trials? This question is just the tip of the iceberg, leading us to a deeper inquiry into the nature of disease, health, and the societal impacts of our immune responses.
In essence, philosophy in the study of immunology encourages us to think critically about the implications of our discoveries. It invites us to reflect on questions such as: What does it mean to be healthy? How do we define disease? And, importantly, what ethical frameworks should guide our research? Each of these questions opens up a dialogue that is not only scientific but also profoundly human, reminding us that at the heart of immunology lies the quest for understanding our very existence and the intricate mechanisms that sustain it.
Understanding the philosophical underpinnings of immunology reveals how concepts like self and non-self shape our comprehension of immune responses and disease mechanisms. These foundational ideas are not merely academic; they have real-world implications for how we approach treatments and vaccinations. The philosophical inquiry into what constitutes the 'self' is crucial, as it informs how we perceive autoimmune diseases, where the body’s defenses mistakenly attack its own cells. This raises profound questions about identity and the very essence of being human. Are we defined solely by our biological makeup, or do our experiences and environments play a role in shaping our immune responses?
Moreover, as we delve deeper, we realize that the implications of these philosophical questions extend beyond individual health. They influence public health strategies, community resilience, and our collective responsibility in combating infectious diseases. In a world increasingly interconnected by travel and trade, understanding the philosophical dimensions of immunology can guide us in crafting policies that protect not just individuals but entire populations.
The ethical considerations surrounding immunological research are critical, impacting decisions on vaccine development, clinical trials, and patient consent. As we venture into the world of immunology, we must grapple with the moral responsibilities that come with scientific inquiry. Are we prioritizing the welfare of participants in our research? Are we transparent about the risks and benefits involved? These questions are essential as they highlight the ethical responsibility researchers have to ensure participant autonomy and welfare.
Informed consent is vital in vaccine trials, ensuring participants understand risks and benefits. It emphasizes the ethical responsibility of researchers to prioritize participant autonomy and welfare. This process is not just a formality; it is a crucial dialogue that respects the individual's right to make informed decisions about their health. Transparency in communication fosters trust, which is essential in building public confidence in vaccines and immunological interventions.
A careful assessment of risks versus benefits in vaccine trials is essential for ethical research. Researchers must engage in transparent and clear communication with participants about potential outcomes, ensuring that individuals can make informed choices. This balancing act is akin to walking a tightrope, where one misstep could lead to ethical dilemmas that undermine the integrity of the research.
Special considerations are necessary when involving vulnerable populations in immunological research. Ensuring protections are in place to prevent exploitation and ensure equitable access to benefits is paramount. Vulnerable groups, including children, the elderly, and marginalized communities, require additional safeguards to ensure their rights and well-being are prioritized. This ethical obligation is a reflection of our values as a society and our commitment to justice and equity in healthcare.
Exploring various philosophical perspectives on disease helps frame our understanding of health, illness, and the social implications of immunological conditions. These perspectives influence public health policies and practices, guiding how we approach disease prevention and treatment. By examining the philosophical dimensions of disease, we can better understand the societal factors that contribute to health disparities and the importance of addressing these issues in our healthcare systems.
The philosophical concept of self is central to immunology, guiding how we define immunity, autoimmune diseases, and the boundaries of the body's defenses against pathogens. This exploration leads us to consider the implications of our understanding of self on health and disease.
Autoimmunity challenges traditional notions of self, raising philosophical questions about identity, agency, and the implications of the immune system attacking the body it is meant to protect. This paradox invites us to reconsider our definitions of health and illness, pushing us to explore the complex interplay between biology and identity.
The societal implications of immunity extend beyond individual health, influencing public health strategies, community resilience, and collective responsibility in combating infectious diseases. Understanding immunity as a shared societal asset can foster a sense of community and encourage collaborative efforts in disease prevention and management.
- What is the role of philosophy in immunology?
Philosophy helps us understand the ethical implications and foundational concepts that shape our approach to immunology. - How does the concept of self impact immunological research?
The concept of self is crucial in defining immunity and understanding autoimmune diseases. - Why is informed consent important in vaccine trials?
Informed consent ensures participants understand the risks and benefits, prioritizing their autonomy and welfare.

The Philosophical Foundations of Immunology
Understanding the philosophical underpinnings of immunology reveals how concepts like self and non-self shape our comprehension of immune responses and disease mechanisms. At its core, immunology is not just a biological science; it is deeply intertwined with philosophical inquiry. The way we define what is considered 'self' versus 'non-self' is not merely a matter of scientific classification but also a profound philosophical question that has implications for how we perceive health and illness.
To illustrate, the immune system's primary function is to distinguish between the body's own cells and foreign invaders, such as bacteria and viruses. This distinction is crucial for maintaining health. However, when the immune system fails to recognize its own cells, it can lead to autoimmune diseases, where the body attacks itself. This raises intriguing philosophical questions about identity and the boundaries of the self. Are we merely a collection of cells, or is there a deeper essence that defines our identity? The philosophical implications of these questions are vast and can shape how we approach treatment and understanding of diseases.
Moreover, the concept of self in immunology can also extend to societal implications. For instance, how do we define the collective 'self' of a community or population in the context of public health? The challenges of infectious diseases require us to think beyond individual immunity and consider the health of the community as a whole. This perspective pushes us to ask: What responsibilities do we have to each other in protecting public health? The answers to these questions often require a philosophical examination of our values, ethics, and societal norms.
In addition, the philosophical foundations of immunology can be seen in the way we approach medical interventions, such as vaccines. The debate surrounding vaccination is not just a scientific one; it is also deeply philosophical. It touches on issues of individual autonomy versus collective responsibility. Should an individual have the right to refuse a vaccine that protects not only themselves but also the community? This tension between personal choice and societal welfare is a classic philosophical dilemma that resonates within the field of immunology.
Ultimately, the philosophical foundations of immunology challenge us to consider not just the mechanics of the immune system but also the broader implications of our understanding of health, identity, and community. By engaging with these philosophical questions, we can enrich our understanding of immunology and its impact on society. As we continue to explore these concepts, it is essential to embrace the complexity and nuance that philosophy brings to the study of immunology.
- What is the significance of the 'self' and 'non-self' concept in immunology? The distinction helps the immune system identify and combat pathogens while maintaining the integrity of the body's own cells.
- How does philosophy influence public health policies? Philosophical inquiries into ethics and responsibility shape how we approach vaccination, disease prevention, and health equity.
- What role do ethical considerations play in immunological research? Ethical considerations ensure that research respects participant autonomy and welfare, particularly in vulnerable populations.

Ethics in Immunological Research
When we delve into the world of immunological research, we encounter a labyrinth of ethical dilemmas that are as complex as the immune systems we study. This field is not just about understanding how our bodies fight off disease; it's also about grappling with profound questions of morality and responsibility. How do we balance the pursuit of knowledge with the need to protect individual rights? What happens when the quest for a cure conflicts with ethical standards? These questions are at the forefront of discussions surrounding vaccine development, clinical trials, and patient consent.
At the heart of these ethical considerations lies the principle of informed consent. This concept is crucial in the realm of vaccine trials, where participants must be fully aware of the risks and benefits involved. Imagine being part of a trial that could potentially save lives, but also carries unknown risks. It's essential for researchers to communicate transparently, ensuring that participants understand what they are getting into. This responsibility to prioritize participant autonomy and welfare is not just a legal obligation; it is a moral imperative that underscores the integrity of the research process.
Informed consent is more than just a form to be signed; it represents a commitment to ethical standards in research. Participants need to be educated about the trial's purpose, the procedures involved, and the potential outcomes. This includes both the benefits that may arise from the research and the risks that could affect their health. Researchers must take the time to explain these factors in a way that is accessible and understandable. After all, how can someone make an informed decision if they don’t fully grasp the implications?
One of the most challenging aspects of immunological research is the delicate act of balancing risks and benefits. Researchers must conduct a thorough assessment of potential hazards against the advantages that the research may provide. This requires a transparent approach where the participants are kept in the loop about possible outcomes. For example, in a vaccine trial, the potential for serious side effects must be weighed against the possibility of developing a vaccine that could save countless lives. This balancing act is not just a scientific endeavor; it is an ethical one that demands careful thought and consideration.
When it comes to immunological research, special considerations are necessary for vulnerable populations. These groups, which may include children, the elderly, or individuals with pre-existing health conditions, require additional protections to prevent exploitation. Researchers must ensure that these populations are not only protected but also have equitable access to the benefits of the research. This raises further questions: How do we ensure that the benefits of immunological advancements reach those who are most in need? And how do we safeguard against the potential for abuse in research practices?
As we navigate through these ethical waters, it becomes clear that the intersection of philosophy and immunology is rich with implications. The decisions made in the lab can resonate far beyond the confines of scientific inquiry, influencing public health policies and the very fabric of society. The ethical landscape of immunological research is a reflection of our values and priorities as a society, and it demands our attention and diligence.
- What is informed consent in immunological research?
Informed consent is the process by which participants are made aware of the risks and benefits of a study, ensuring they can make educated decisions about their involvement. - Why is ethical research important?
Ethical research protects participants' rights and well-being, ensuring that scientific advancements do not come at the expense of individual autonomy. - How do researchers balance risks and benefits?
This is achieved through thorough assessments and transparent communication with participants regarding potential outcomes. - What protections are in place for vulnerable populations?
Researchers must implement additional safeguards to ensure that vulnerable groups are not exploited and have equitable access to research benefits.

Informed Consent in Vaccine Trials
Informed consent is not just a formality in vaccine trials; it is a fundamental ethical principle that ensures participants are fully aware of what they are signing up for. Think of it as the foundation of trust between researchers and participants. Without this trust, the entire framework of clinical research could crumble. Participants must be provided with comprehensive information about the trial, including its purpose, procedures, potential risks, and benefits. This transparency is crucial because it empowers individuals to make informed decisions about their health and well-being.
Imagine walking into a restaurant without knowing the menu or the ingredients of the dishes being served. You wouldn't feel comfortable ordering, right? Similarly, in the context of vaccine trials, participants should never feel like they are in the dark. They need to understand the implications of their involvement. Researchers have a moral responsibility to prioritize participant autonomy and welfare, ensuring that every individual feels respected and valued throughout the process.
Moreover, informed consent goes beyond just signing a piece of paper; it involves ongoing communication. Participants should feel free to ask questions and express concerns at any point during the trial. This dialogue fosters a sense of partnership between researchers and participants, creating an environment where individuals feel safe and supported. For instance, if someone is hesitant about a potential side effect, researchers should be prepared to discuss it openly, providing clear and honest answers.
To break it down further, here are some key elements that should be included in the informed consent process:
- Trial Purpose: Clear explanation of the research goals.
- Procedures: Detailed description of what participation entails.
- Risks: An honest assessment of potential side effects or complications.
- Benefits: Information on what participants might gain from being involved.
- Confidentiality: Assurance that personal data will be protected.
In addition, it is essential to ensure that the language used in consent forms is accessible to all participants. Avoiding complex medical jargon can make a significant difference in comprehension. Researchers should strive to present information in a way that is straightforward and relatable, helping participants to grasp the concepts without feeling overwhelmed.
Ultimately, informed consent is not just a checkbox; it is a commitment to ethical research practices. It reflects a respect for individual autonomy and acknowledges the importance of participant welfare in the pursuit of scientific knowledge. As we continue to advance in immunological research, fostering an environment where informed consent is prioritized will be crucial in building a more ethical and trustworthy research landscape.
- What is informed consent? It is the process of providing participants with comprehensive information about a clinical trial, ensuring they understand the risks and benefits before agreeing to participate.
- Why is informed consent important? It respects the autonomy of participants and ensures they make educated decisions regarding their health and involvement in research.
- Can participants withdraw from a trial? Yes, participants have the right to withdraw from a trial at any time without any penalty.
- How is participant confidentiality maintained? Researchers are required to protect personal data and ensure that it is used solely for research purposes.

Balancing Risks and Benefits
In the realm of immunological research, particularly during vaccine trials, the process of is not just a procedural necessity; it is a profound ethical obligation. Researchers are tasked with the critical challenge of ensuring that the potential benefits of a vaccine outweigh the risks involved in its administration. This balance is essential for fostering trust and transparency between the research community and the public. Imagine a tightrope walker, carefully navigating the delicate line between safety and innovation; this is akin to how researchers must approach their work.
To achieve this balance, a comprehensive assessment of both the risks associated with the vaccine and the potential benefits to public health must be conducted. For instance, while a vaccine might carry certain side effects, the overarching goal is to prevent a disease that could lead to severe health complications or even death. This is where the concept of informed consent plays a pivotal role. Participants in vaccine trials must be made fully aware of any risks they may encounter, as well as the potential benefits not just for themselves, but for society at large.
Moreover, researchers must engage in transparent communication with participants, providing them with clear, accessible information. This includes details about the nature of the vaccine, the methodology of the trial, and the anticipated outcomes. In many cases, the risks might be minimal compared to the potential for widespread immunity against a contagious disease. For example, consider the following table that illustrates a hypothetical risk-benefit analysis for a new vaccine:
| Aspect | Risks | Benefits |
|---|---|---|
| Side Effects | Mild fever, fatigue | Prevention of severe illness |
| Long-term Effects | Unknown | Herd immunity |
| Public Perception | Vaccine hesitancy | Community health improvement |
This table serves to highlight the multifaceted considerations that researchers must weigh. While the risks may seem daunting, the potential benefits can be life-saving, not only for individuals but for entire communities. The ethical responsibility of researchers extends beyond just conducting trials; it encompasses a duty to educate and inform the public, ensuring that individuals can make well-informed decisions regarding their participation.
Ultimately, the goal is to cultivate a culture of ethical research that prioritizes participant welfare while advancing scientific knowledge. By maintaining this balance, researchers can contribute to a future where vaccines are not only effective but also embraced by the communities they aim to protect. In this ongoing dialogue between science and ethics, the voices of participants must be heard, ensuring that the path forward is not just scientifically sound, but also socially just.
- What are the primary risks associated with vaccine trials? Risks can include mild side effects like fever or fatigue, and in rare cases, more severe reactions.
- How are participants informed about these risks? Participants receive detailed information during the informed consent process, which outlines potential risks and benefits.
- Why is balancing risks and benefits important? It ensures ethical standards are met, fostering trust and safety in the research process.
- What role does public perception play in vaccine trials? Public perception can influence participation rates and overall success, making communication vital.

Vulnerable Populations in Research
When it comes to immunological research, the inclusion of vulnerable populations requires a delicate balance of ethical considerations and scientific rigor. Vulnerable groups, such as children, the elderly, pregnant women, and individuals with compromised health, often face a higher risk of exploitation in clinical trials. This raises important questions: How can we ensure their protection while advancing scientific knowledge? What measures are in place to safeguard their rights and well-being?
To address these concerns, researchers must implement strict guidelines that prioritize the autonomy and welfare of participants. This includes obtaining informed consent that is not only clear but also comprehensible. Participants should fully understand the potential risks and benefits associated with their involvement in research. For instance, a study involving a new vaccine must clearly communicate the possible side effects alongside the benefits of immunity it offers.
Moreover, the ethical treatment of vulnerable populations goes beyond mere consent; it encompasses the entire research process. Researchers should consider the unique circumstances that these groups face. For example, when conducting trials with children, special attention must be given to their understanding and willingness to participate. It's crucial to engage parents or guardians in the decision-making process, ensuring that children are not coerced into participating.
Additionally, researchers should be aware of the potential for power imbalances in these situations. Vulnerable populations may feel pressured to participate due to socioeconomic factors or a lack of access to healthcare. To mitigate this, ethical guidelines must mandate equitable recruitment practices that do not exploit these individuals. This means ensuring that the benefits of research, such as access to new treatments or vaccines, are distributed fairly and do not disproportionately favor certain groups over others.
Ultimately, the goal of including vulnerable populations in immunological research should be to enhance our understanding of diseases and improve health outcomes for everyone. By fostering an environment of trust and respect, researchers can ensure that these populations are not just subjects of study but active participants in the advancement of medical science. This commitment to ethical integrity not only protects vulnerable groups but also enriches the research, leading to more comprehensive and applicable findings.
- What defines a vulnerable population in research? Vulnerable populations are groups that may have limited autonomy or heightened risk of exploitation in research settings, such as children, the elderly, or those with disabilities.
- How is informed consent obtained from vulnerable populations? Informed consent involves providing clear and comprehensive information about the study, ensuring that participants (and their guardians, if applicable) understand the risks and benefits before agreeing to participate.
- What protections are in place for vulnerable populations in research? Ethical guidelines and regulations are designed to protect vulnerable populations, including oversight by institutional review boards (IRBs) and requirements for equitable recruitment practices.
- Why is it important to include vulnerable populations in immunological research? Including these groups helps ensure that research findings are applicable to all segments of the population, leading to better health outcomes and more effective treatments.

Philosophical Perspectives on Disease
When we delve into the , we find ourselves navigating a complex landscape that intertwines health, illness, and societal implications. It's fascinating how our understanding of disease is not merely a biological phenomenon but also a deeply philosophical one. At its core, disease challenges our notions of what it means to be human. It raises questions about our identity, our agency, and even our morality. For instance, consider the age-old debate about whether disease is a punishment, a test, or simply a part of the human experience. This philosophical inquiry can significantly shape public health policies and practices.
Moreover, the way we conceptualize disease influences how we respond to it as a society. Do we view it as an individual failing, or do we recognize the broader social determinants that contribute to health disparities? This perspective is crucial, especially in addressing issues such as access to healthcare and social justice. By understanding disease through a philosophical lens, we can better appreciate the interconnectedness of our health and the health of our communities.
One interesting aspect of philosophical perspectives on disease is the distinction between acute and chronic conditions. Acute diseases, like the flu, often prompt immediate and collective responses, while chronic diseases, such as diabetes, can lead to a more individualistic approach. This dichotomy can be reflected in public health strategies and funding allocations. For example, consider the following table that outlines the differences:
| Aspect | Acute Disease | Chronic Disease |
|---|---|---|
| Duration | Short-term | Long-term |
| Response | Immediate | Ongoing |
| Public Perception | Collective concern | Individual responsibility |
| Healthcare Approach | Emergency services | Chronic management |
This table illustrates how our perceptions can influence healthcare approaches. The philosophical inquiry into disease also opens up discussions about the implications of labeling individuals as "sick" or "healthy." These labels can carry significant weight, affecting how individuals view themselves and how society perceives them. The stigma surrounding certain diseases can lead to isolation, discrimination, and a lack of support, which only exacerbates the challenges faced by those living with illness.
Furthermore, the philosophical exploration of disease extends to the ethical implications of treatment and research. Questions arise about the value of life and the moral obligations we have to those who are ill. For instance, should resources be allocated to treat all diseases equally, or should we prioritize based on severity, prevalence, or societal impact? These discussions are vital as they inform not only healthcare policies but also our collective values as a society.
In conclusion, the philosophical perspectives on disease challenge us to reflect on our values, beliefs, and societal structures. They compel us to consider the broader implications of health and illness, prompting discussions that can lead to more equitable and just healthcare systems. By embracing this philosophical inquiry, we can foster a more compassionate society that values health as a shared responsibility.
- What role does philosophy play in understanding disease?
Philosophy helps us explore the deeper implications of disease, including ethical, social, and personal dimensions that go beyond biological factors. - How can philosophical perspectives influence public health policy?
By examining the values and beliefs underlying health issues, philosophical perspectives can guide more equitable and effective public health strategies. - Why is it important to consider the social implications of disease?
Understanding the social determinants of health can help address disparities and promote a more inclusive approach to healthcare. - What is the significance of the acute vs. chronic disease distinction?
This distinction influences how we allocate resources and develop public health responses, affecting both individual and community health outcomes.

Immunology and the Concept of Self
Understanding immunology through the lens of the concept of self is like trying to solve a complex puzzle where each piece represents a different aspect of our body's defenses. At its core, immunology is the study of how our immune system distinguishes between what is part of our body and what is foreign. This distinction is crucial, as it determines how we respond to pathogens like bacteria and viruses. The philosophical implications of this concept are profound, as they not only shape our understanding of immunity but also influence how we perceive health, illness, and our very identity.
When we think about the immune system, we often envision it as a vigilant guardian, constantly on the lookout for intruders. However, this guardian must also recognize its own citizens—our cells and tissues. This is where the idea of self becomes pivotal. The immune system employs a variety of mechanisms to identify self from non-self, a process that can be likened to a security system that has to differentiate between a family member and an intruder. If it fails in this regard, the consequences can be dire, leading to autoimmune diseases where the body mistakenly attacks its own cells.
Autoimmunity raises fascinating questions about the nature of identity and agency. For instance, if the immune system is attacking what it perceives as a threat within the body, how does this affect our understanding of self? Are we still the same person if our immune system is at war with our own tissues? This philosophical dilemma invites us to reconsider our definitions of health and illness. It challenges the binary notion of self and other, suggesting that the boundaries of identity might be more porous than we previously thought.
Furthermore, the implications of these philosophical inquiries extend beyond individual health. They influence public health policies and community approaches to disease management. For example, consider how society reacts to outbreaks of infectious diseases. The concept of collective immunity, or herd immunity, underscores the idea that individual health is interconnected with the health of the community. This realization compels us to think about our responsibilities towards one another, especially in the face of global health challenges.
In summary, the interplay between immunology and the concept of self is a rich field of inquiry that invites us to explore not just the biological mechanisms at play but also the philosophical and ethical dimensions of our understanding of health and identity. As we continue to unravel the complexities of the immune system, we must also reflect on how these insights shape our perceptions of ourselves and our relationships with others in society.
- What is the concept of self in immunology? The concept of self in immunology refers to the immune system's ability to recognize and differentiate between the body's own cells and foreign pathogens.
- How does autoimmunity affect our understanding of identity? Autoimmunity challenges traditional notions of identity by raising questions about how we define ourselves when our immune system attacks our own body.
- What are the societal implications of immunity? The societal implications of immunity include the need for collective responsibility in disease prevention and the impact of public health strategies on community health.

Autoimmunity and Identity
Autoimmunity is a fascinating yet perplexing phenomenon that challenges our fundamental understanding of identity and the self. At its core, autoimmunity occurs when the immune system mistakenly identifies the body's own cells as foreign invaders, leading to a self-destructive response. This raises profound philosophical questions: What does it mean to be 'self'? How do we reconcile the idea of a protective immune system with the reality of it attacking its host? These questions not only delve into the biological mechanisms but also touch on deeper existential themes.
To illustrate this, consider the immune system as a vigilant guardian, trained to distinguish between friend and foe. However, in the case of autoimmunity, this guardian becomes confused, turning against its own. This transformation prompts us to reflect on the nature of identity itself. Are we merely a collection of biological processes, or is there a more profound essence that defines who we are? The struggle between self and non-self in autoimmunity forces us to confront the fluidity of identity, suggesting that it is not a fixed state but rather a dynamic interplay influenced by various factors, including genetics, environment, and even philosophical beliefs.
Moreover, the implications of autoimmunity extend beyond individual health; they ripple through our understanding of community and societal identity. When individuals experience autoimmune diseases, they often face not only physical challenges but also social stigma and isolation. This brings to light the interconnectedness of health and identity. For instance, someone with lupus may find their identity reshaped by their condition, prompting shifts in how they view themselves and how they are perceived by others.
In grappling with these complex issues, it is essential to recognize the psychological and emotional dimensions of autoimmunity. Many individuals report feelings of betrayal by their own bodies, leading to a crisis of identity. This inner turmoil can manifest in various ways, impacting mental health and overall well-being. Understanding autoimmunity through a philosophical lens allows us to appreciate the broader implications of how we define ourselves in relation to our health.
Furthermore, the philosophical discourse surrounding autoimmunity can inform public health strategies and healthcare practices. By acknowledging the identity struggles faced by those with autoimmune conditions, healthcare providers can foster a more empathetic and holistic approach to treatment. This perspective encourages the integration of psychological support alongside medical interventions, ultimately promoting a more comprehensive understanding of health that encompasses both the physical and emotional aspects of living with autoimmune diseases.
In conclusion, the intersection of autoimmunity and identity is a rich field for exploration, inviting us to rethink our definitions of self and the implications of our biological systems. As we continue to study these phenomena, we must remain open to the philosophical inquiries that challenge our perceptions and deepen our understanding of what it means to be human.
- What is autoimmunity? Autoimmunity occurs when the immune system mistakenly attacks the body's own cells, leading to various autoimmune diseases.
- How does autoimmunity affect identity? Autoimmunity can challenge individuals' perceptions of themselves, as they navigate the complexities of living with a condition that targets their own bodies.
- Can philosophical perspectives help in understanding autoimmunity? Yes, philosophical inquiries can provide insights into the nature of self, identity, and the emotional impacts of living with autoimmune diseases.
- What role does mental health play in autoimmunity? Mental health is crucial, as individuals with autoimmune conditions may experience feelings of betrayal and isolation, affecting their overall well-being.

Immunity in the Context of Society
When we think about immunity, it’s easy to get lost in the science of it all—the cells, the antibodies, the complex interactions that happen within our bodies. However, the reality is that immunity doesn’t exist in a vacuum; it’s deeply intertwined with society. Just as a tree doesn’t grow in isolation, our immune responses are affected by the environment, culture, and community around us. Understanding this relationship is crucial, especially when we consider how we tackle public health challenges.
The concept of immunity extends beyond individual health; it embodies a collective responsibility. In a society where infectious diseases can spread like wildfire, the health of one person can significantly impact the health of many. For instance, when a significant portion of the population is vaccinated, herd immunity is achieved. This phenomenon protects those who cannot be vaccinated—such as infants and individuals with certain medical conditions—by reducing the overall amount of the virus or bacteria in the community. This interconnectedness highlights the importance of vaccination programs and public health initiatives.
Moreover, the societal implications of immunity become even more pronounced in times of crisis, such as during pandemics. The COVID-19 pandemic, for example, revealed how interconnected our health is and how quickly misinformation can spread. The collective response to the pandemic demonstrated the need for clear communication and public trust in health authorities. This situation raised ethical questions about access to vaccines, the prioritization of groups, and the balance between individual rights and community health. It’s a fine line to walk, and the philosophical implications are profound.
In addition, we must consider how social determinants of health—like socioeconomic status, education, and access to healthcare—affect immunity. People from marginalized communities often face barriers that can lead to poorer health outcomes. For example, limited access to healthcare services can result in lower vaccination rates, making these communities more vulnerable to outbreaks. Addressing these disparities is not just a matter of health; it’s a matter of justice and equity.
As we navigate these complex issues, it’s essential to foster an inclusive dialogue that brings together various stakeholders—health professionals, policymakers, and the community at large. We must ask ourselves: How can we create a society that prioritizes health for all? How do we ensure that everyone has access to the resources they need to maintain their immunity? These questions are not just theoretical; they are practical challenges that require urgent attention.
In conclusion, immunity is not solely a biological concept; it is a social construct that reflects our values, priorities, and responsibilities as a community. By embracing this holistic perspective, we can work towards a healthier society where everyone has the opportunity to thrive. After all, as the saying goes, “It takes a village.” In the realm of health, this couldn’t be more true.
- What is herd immunity? Herd immunity occurs when a significant portion of a population becomes immune to a disease, reducing its spread and protecting those who are not immune.
- Why is public health important in the context of immunity? Public health initiatives, such as vaccination programs, help protect entire communities from infectious diseases, ensuring collective safety and well-being.
- How do social determinants affect immunity? Factors like socioeconomic status, education, and access to healthcare can significantly influence an individual's health outcomes and susceptibility to diseases.
- What role does misinformation play in public health? Misinformation can undermine trust in health authorities and lead to poor health decisions, affecting community immunity and overall health.
Frequently Asked Questions
- What is the relationship between philosophy and immunology?
Philosophy and immunology intersect in fascinating ways. Philosophical concepts, such as the ideas of self and non-self, play a crucial role in shaping our understanding of how the immune system functions. By examining these philosophical foundations, we can gain deeper insights into the mechanisms of disease and the ethical implications of immunological research.
- Why is informed consent important in vaccine trials?
Informed consent is a cornerstone of ethical research, particularly in vaccine trials. It ensures that participants are fully aware of the risks and benefits involved, allowing them to make educated decisions about their participation. Researchers have a moral responsibility to prioritize participant autonomy and welfare, making transparency and clear communication essential.
- How do ethical considerations affect immunological research?
Ethical considerations are paramount in immunological research, influencing various aspects such as vaccine development and clinical trials. These considerations raise questions about moral responsibility, societal implications, and the need to protect vulnerable populations. Researchers must navigate these ethical waters carefully to ensure that their work benefits society while respecting individual rights.
- What are the implications of autoimmunity on our understanding of self?
Autoimmunity challenges traditional notions of self by presenting scenarios where the immune system mistakenly attacks the body it is designed to protect. This raises profound philosophical questions about identity, agency, and the boundaries of our immune defenses. Understanding autoimmunity can reshape our perspectives on health, illness, and the very concept of what it means to be human.
- How does society influence immunity and public health strategies?
The societal implications of immunity extend far beyond individual health. They play a crucial role in shaping public health strategies and community resilience. Collective responsibility in combating infectious diseases is vital, as it fosters a sense of unity and cooperation among individuals, ultimately leading to healthier communities.
- What special considerations are there for vulnerable populations in immunological research?
When involving vulnerable populations in immunological research, special considerations are necessary to prevent exploitation and ensure equitable access to benefits. Researchers must implement robust protections and ethical guidelines to safeguard these individuals, ensuring that their rights and welfare are prioritized throughout the research process.